The healthcare industry produces more than a third of the world’s digital information. Analysts project global data creation will reach 180 zettabytes by 2025. Yet nearly all of that information remains unused – rendered unintelligible by incompatible formats and scattered databases.
Artificial intelligence (AI) can unlock this treasure trove by extracting insights from unstructured patient data, images, genetics, genomics, labs, and more. At GE HealthCare, we are leveraging AI to increase efficiencies on the device through solutions like AIR Recon DL and Sonic DL, in the patient care journey with offerings like Caption AI, and in operational intelligence across the enterprise with Command Center.
We’ve seen in very real ways how AI can address some of the most complex challenges in healthcare. However, ultimately it is important to remember that the technologies that fall under the umbrella of artificial intelligence are not infallible. Just as human clinicians can make mistakes, AI systems can too, which is why we must carefully manage uncertainty in both cases.
In order to reap the benefits of AI, clinical and technology practitioners have to be responsible and intentional in how to use these technologies. The five practices below offer a framework for deploying AI thoughtfully, safely, and at scale.
- Pick a problem and set clear goals
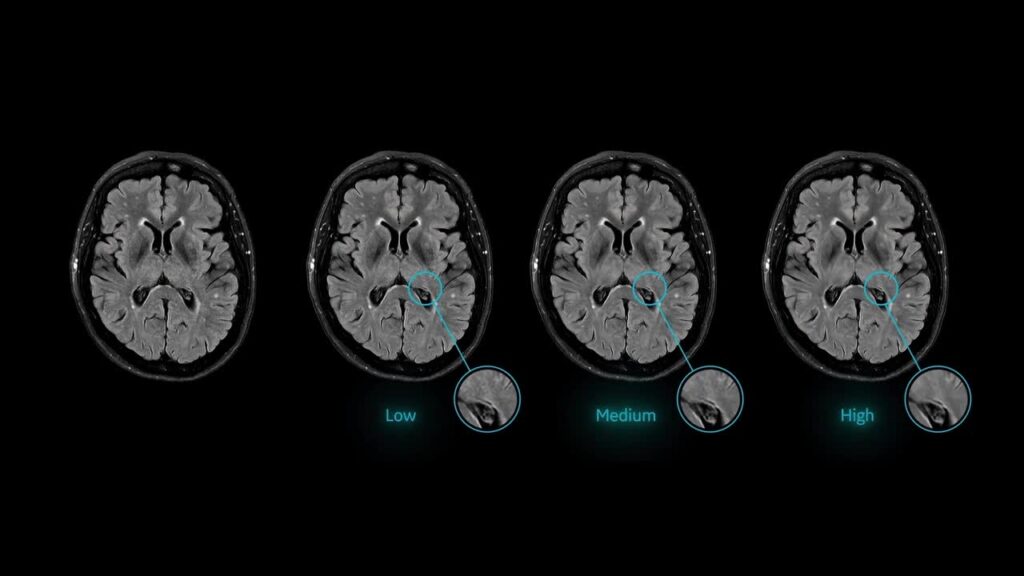
Begin by identifying the most pressing pain points for patients and providers, then establish a clear, concise set of measurable goals that AI can help achieve. Treat AI as a means to address specific challenges, not as an objective in itself. Take the example of magnetic resonance imaging (MRI), where longer scan times can be more expensive for the provider and incredibly frustrating for the patient. These problems are further compounded on occasions where the quality of the scan is compromised, necessitating a repeat visit. We developed AIR Recon DL to address this specific problem. AIR Recon DL can improve MRI scan times by up to 50%, which increases the number of scans that can be completed in addition to improving the patient experience.[1] In addition, the solution also sharpens images by 60%, reducing the risk of rescan.[2]
To take another example, delays in bed assignment time at hospitals can drive inefficiencies in bed usage, poor patient experience, and lower quality of care. Duke Health prioritized the resolution of this issue with GE HealthCare Command Center (an AI-powered solution that transforms complex hospital data into actionable insights, enabling proactive staffing and resource planning to better enable the right staff to be in the right place at the right time). The clear focus on the problem to be solved helped Duke decrease bed request to bed assigned time by 66%, and reduced temporary labor requirements by 50%.[3] - Choose one or more partners who fit your needs
There are a wide variety of problems to tackle in the healthcare industry, and it will take a community to solve all of them. That’s why choosing the right AI vendor—or vendors—is about more than just technology. While a single-vendor approach can simplify integration and reduce complexity, a multi-vendor strategy allows organizations to tap into specialized innovations, adapt quickly to emerging needs, and reduce dependency on any one provider. Startups bring agility and speed to new applications, though they may face hurdles with scale or regulation. On the flip side, established firms offer proven stability and regulatory experience. The most effective strategy often blends both – prioritizing partners who demonstrate flexibility, scalability, and a strong cultural alignment with your mission. While making your choices, select vendors who are committed to working collaboratively within a broader ecosystem to drive long-term impact. - Keep humans involved at every step
AI is not infallible, which is why human oversight is essential to ensure safety and build trust. Before deploying any model, teams should rigorously test its outputs against historical clinical data to confirm accuracy. After deployment, it’s important to evaluate the specific use case to determine the most appropriate level of human involvement. For example, for the use case of allocating beds automatically at hospitals – a feature of Command Center – you might begin with a human approver in the loop, then transition to full automation once confidence in the model is established. In contrast, for clinical decisions like those made in a virtual tumor board—as demonstrated with Health Companion[4], an agentic AI system under development that is aimed at providing multi-disciplinary expertise through specialized agents—a provider should always make the final call. Regardless of the approach, a review committee should regularly audit both random and high-risk cases to detect performance drift. This approach can better ensure the model remains aligned with clinical practice.
This is especially important as clinician feedback plays a key role in refining AI behavior. Through reinforcement learning, providers can rate or correct AI-generated outputs, helping the system evolve toward expert-level performance. To support transparency, institutions should use explainability tools that can help show the data that influenced each prediction. Visual grounding can link report statements to specific areas in medical images, while ontology-based frameworks ensure consistent medical terminology and logical coherence. For generative AI, applying temperature controls helps limit randomness and maintain reliable outputs.
- Monitor performance with reliable reference data
Monitoring your AI is critical to ensure it continues to perform accurately and safely over time. As clinical environments and patient data evolve, models can drift, leading to reduced effectiveness or unintended errors. Ongoing oversight helps catch these issues early, supports continuous improvement through clinician feedback, and builds trust among users. It also is consistent with regulatory standards and ethical expectations, which are especially important in healthcare.
Ultimately, monitoring transforms AI from a static tool into a dynamic, reliable partner in delivering high-quality care. Techniques like pseudo-label discrepancy (SUDO) can flag ambiguous cases for human review, a key factor of ensuring reliability.
5. Integrate AI into daily work seamlessly
Integrating AI into the clinical workflow is essential because clinicians are already overburdened, and asking them to manage yet another screen or tool is a non-starter. To maximize effectiveness, AI must be seamless—the ideal scenario is one that requires zero clicks—and embedded directly into the tools clinicians already use. For example, on-device AI like Sonic DL can improve cardiac MRI scan times by up to 83%[5] compared to fully sampled MR datasets, without any additional input from the user. Similarly, Caption AI technology on the Vscan Air SL handheld ultrasound provides real-time, step-by-step guidance to help clinicians capture diagnostic-quality cardiac images, and automatically estimate ejection fraction, right at the point of care. These kinds of frictionless integrations not only enhance efficiency and decision-making, but also increase adoption by fitting naturally into the clinical routine.
Successfully deploying AI in healthcare isn’t about chasing the latest technology—it’s about solving real problems with purpose, precision, and partnership. The five steps outlined here provide a practical roadmap for doing just that: starting with clear goals, choosing the right collaborators, keeping humans in the loop, monitoring performance, and integrating AI seamlessly into daily workflows. When done thoughtfully, AI becomes more than a tool—it becomes a trusted partner in delivering safer, faster, and more personalized care. As the healthcare landscape continues to evolve, organizations that take a measured, responsible approach to AI will be best positioned to lead the way. The future of healthcare will be shaped not just by innovation, but by how wisely and collaboratively we put that innovation to work.
[1] https://www.gehealthcare.com/products/magnetic-resonance-imaging/air-recon-dl?srsltid=AfmBOorgUf2IuxhVreAuJiUAC-i7gPfXBOkBZOfiwEi5PwxB8VOcnMkn
[2] https://www.gehealthcare.com/products/magnetic-resonance-imaging/air-recon-dl?srsltid=AfmBOorgUf2IuxhVreAuJiUAC-i7gPfXBOkBZOfiwEi5PwxB8VOcnMkn
[3] https://www.gehccommandcenter.com/2025-outcomes-source-data
[4] Concept only. This work is in concept phase and may never become a product. Not for Sale. Any reported results are preliminary and subject to change. Not cleared or approved by the U.S. FDA or any other global regulator for commercial availability.
[5] https://www.gehealthcare.com/about/newsroom/press-releases/ge-healthcare-introduces-sonic-dl-a-groundbreaking-fda-cleared-ai-deep-learning-technology-for-faster-mri?npclid=botnpclid&srsltid=AfmBOooqIxg5yAQPj7PcxsfJlYj9doixCKlPJo1Nq9jimkGd5JJjR3xe



