Healthcare is one of the most complex operating systems in the world. Even when occupancy looks steady, the ground is constantly shifting. With a national average length of stay of about 4.7 days1, a typical hospital effectively “turns” one in five beds every day as admissions, discharges, and transfers reshape demand by the hour.
That volatility meets rising complexity. Patient acuity and case-mix have steadily increased, leaving hospitals to care for sicker patients as lower-acuity care moves to outpatient settings2. Each hospitalization can involve 15–20 different providers—physicians, nurses, therapists, pharmacists, transporters, and others—whose work must align in real time across multiple departments.
Layer on workforce churn and the challenge multiplies. Hospital staff turnover now averages roughly 18% a year3, forcing constant adjustments to scheduling, coverage, and training.
In this environment, even small operational changes can have outsized effects.
- Opening an observation unit can shift nurse and tech staffing and alter downstream bed availability.
- Adjusting OR block schedules can change PACU throughput, ICU demand, and ED boarding risk.
- Adding ICU beds can cascade through step-down, telemetry, and transport capacity.
Traditional planning tools, which are built on “average” length of stay, “average” acuity, and “average” demand, can’t keep up. In a hospital, there is no such thing as average.
That’s why GE HealthCare built the Digital Twin—an industrial-grade simulation engine designed specifically for hospitals and health systems.
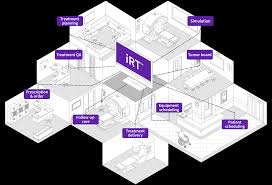
A Digital Twin in healthcare is a virtual model that simulates real-life patient and staff behavior, variations in demand and supply, and complex patient pathways. It empowers hospital leaders to make data-driven decisions by testing different scenarios in a safe, digital environment.
Through this kind of modeling, hospitals can explore how operational changes such as capacity planning, resource allocation, facility design, or staffing strategies ripple across the system. Whether leaders are preparing for seasonal surges, evaluating new construction, or optimizing existing workflows, the Digital Twin translates “what if” questions into measurable projected outcomes.
In short, it transforms how hospitals plan, predict, and perform, turning complexity into clarity and insight into action.

Why Generic Models Fall Short
Discrete-event simulation has been used in industries like manufacturing and logistics for decades. But applying those models directly to healthcare is problematic. Unlike assembly lines, hospitals deal with:
- Variability: Patient arrivals fluctuate unpredictably, from seasonal pediatric surges to trauma cases.
- Interdependence: The effects of a discharge delay on one floor can cascade to the ED, OR, and post-acute units.
- Dynamic environments: Staffing, acuity, and bed availability change by the minute.
Generic models typically assume static or average values. In healthcare, this leads to misleading results and a false sense of confidence in plans that won’t hold up under real conditions.
The GE HealthCare Digital Twin was engineered to capture healthcare’s true statistical behavior, so that simulations mirror real-world dynamics.
What Makes It Different
The Digital Twin’s power lies in four attributes designed for healthcare:
- Speed – Hospitals can be modeled in months, not years. This allows leaders to run scenarios and make decisions while conditions are still relevant.
- Modularity – Hospitals can begin modeling at either end of the spectrum: micro (a single ED, OR, or unit) or macro (an entire hospital or multi-hospital system). The model can then expand in either direction, layering insights from unit-level detail to system-wide dynamics.
- Longevity – With data updates every 6–12 months, a Digital Twin can serve as a reusable planning tool for years, not just a single project.
- Dynamic Simulation – Instead of relying on averages, the model learns the statistical behaviors of patients, staff, and resources so simulations are realistic and actionable.
A Six-Phase Methodology
Developing a Digital Twin is as much about governance and stakeholder alignment as it is about modeling. This data-driven, collaborative planning process is designed to deliver results in less than six months:
- Launch & Governance – Establish goals, form a steering committee, and set up communication and decision-making structures.
- Assessment – Gather retrospective data, document workflows, and interview stakeholders to capture operational realities.
- Scenario Framework – Define the “what if” questions, such as: Should we build a new tower or reallocate existing capacity? Should we change surgical schedules?
- Iterative Modeling – Build and refine simulations, test multiple scenarios, and measure tradeoffs.
- Recommendations – Present data-driven insights, showing leaders the impact of different paths.
- Go-Forward Plan – Deliver a roadmap with priorities, accountability, and next steps.
This methodology transforms the Digital Twin from a one-off model into a decision-support system that organizations can rely on repeatedly.
Technology in Action
The best way to understand the Digital Twin is to see how it works in practice. Across hospitals and health systems, it can be applied to challenges ranging from seasonal surge planning to command center design, capital investment decisions, and surgical scheduling. Each example highlights how simulation translates complexity into clarity and why a purpose-built model for healthcare delivers insights that generic models simply can’t match.
1. Preparing for Seasonal Surges
Pediatric hospitals face sharp seasonal spikes in respiratory illness. Using Digital Twin, Children’s Mercy Kansas City can forecast when surges will hit, what diagnoses are likely to dominate, and what resources will be needed.
Instead of reacting when the ED is already overflowing, the hospital can preemptively open beds, onboard additional staff, and ensure the right resources are available. “It’s important that we’re prepared for surges, and the Digital Twin has been remarkable in helping us do that,” said Stephanie Meyer, Senior Vice President and Chief Nursing Officer at Children’s Mercy Kansas City.
2. Deciding on Expansion vs. Optimization
For many systems, the core question is whether to build new capacity or unlock more from the existing footprint. A Digital Twin can compare both paths side by side using the system’s own data. Leaders can test scenarios such as adding a tower, reconfiguring bed types, consolidating low-volume units, or decanting observation patients to a dedicated unit. The model projects impacts on access and flow (admissions served, ED boarding hours, transfer acceptance), patient experience (waits to bed, cancellations), staffing (FTE requirements, skill mix, overtime exposure), and cost (capital outlay, operating expense).
By quantifying tradeoffs, such as “optimize now” vs. “build later,” executives see which option delivers the best return for access, quality, and financial performance.
3. Optimizing Surgical Schedules
Operating rooms set the tempo for the whole hospital. The Digital Twin evaluates alternative block allocations, add-on rules, case sequencing, and turnover practices, then forecasts downstream effects on PACU holds, ICU bed demand, step-down capacity, and inpatient census.
It also estimates operational KPIs such as on-time starts, block utilization, case throughput, late-day overages, and staffing coverage by role. Hospitals can test questions like: What if we shift cardiac blocks earlier? What if ortho runs longer lists on fewer days? What if we cap add-ons after a certain hour?
The model reveals where bottlenecks will form and which schedule yields the best balance of throughput, safety, and staffing feasibility.
4. Redesigning Units and Departments
Physical layouts can have a dramatic impact on patient flow and staff efficiency. The distance between rooms, placement of supply areas, and visibility of patients all influence how quickly teams can respond and complete care tasks. In one recent hospital redesign study, nurses were found to walk an average of 1.8 miles per shift4, a clear reminder that even well-intentioned layouts can create hidden inefficiencies and fatigue.
Before construction begins, Digital Twin simulations allow leaders to test proposed footprints and workflows, projecting how different layouts will affect throughput, care delivery, and team performance. The result is design choices grounded in data rather than assumptions. That helps organizations create environments that work as well operationally as they do architecturally.
5. Balancing Programs Across a Network
In multi-hospital systems, deciding where services should live is a system-wide puzzle. The Digital Twin models options such as opening observation units, concentrating stroke care, or redistributing surgical specialties to show how each decision impacts access, travel time, and utilization across the network. It also projects staffing implications (coverage by specialty, call burden, transport demand) and operational outcomes (ED load leveling, elective case growth, post-acute flow). Leaders can compare opportunities like centralizing a service at one hub versus creating two regional centers and see which configuration improves access while keeping each site stable and sustainable.
The Bottom Line
Healthcare leaders don’t have the luxury of trial and error. A poorly informed decision can lead to wasted capital, staff burnout, and reduced patient access. The Digital Twin provides:
- A shared reality for diverse stakeholders so high-stakes decisions aren’t based on subjective and often conflicting viewpoints.
- Faster iteration so systems can test dozens of scenarios before acting.
- Evidence-based recommendations that align operations with strategic goals.
It’s not just about modeling hospitals. It’s about building a future where every major healthcare decision is tested, measured, and informed by accurate, data-driven projections.
Check out the Executive Brief “Capacity Strategy Powered by a Digital Twin: Examining Use Case Scenarios” to learn more about the research and technology powering GE HealthCare’s Digital Twin and how it’s helping providers design the future of hospital operations.
- https://www.definitivehc.com/resources/healthcare-insights/average-length-of-stay-by-state ↩︎
- https://www.aha.org/guidesreports/2024-05-01-2023-costs-caring ↩︎
- https://www.nsinursingsolutions.com/documents/library/nsi_national_health_care_retention_report.pdf ↩︎
- https://www.hfmmagazine.com/articles/5018-using-data-to-optimize-inpatient-environments ↩︎