The first cry of a newborn can silence even the busiest hospital unit: a brief, luminous pause when everyone in the room remembers why they chose this work. Yet in the moments leading up to the first cry prior to birth, a subtler chorus begins: fetal monitor tracings ebb and flow across glass, drip rates tick on infusion pumps, maternal vital signs accumulate line by line. Within seconds, the poetry of birth collides with a blizzard of data.
That data does not always play out in a neat formation. Nurses, physicians, and the unseen IT guardians who keep the monitors running navigate a maze of login prompts, clicks, printouts, and screens that seldom speak the same language. What should feel like choreography often plays out as traffic, with each clinician searching for the right readout.
These moments of transition expose a deeper truth: every role at the heart of labor and delivery faces a different kind of pressure. Despite medical advances, maternal and fetal risks remain a critical challenge: the U.S. ranks 65th among industrialized nations in maternal deaths1, and has the highest rates of maternal and fetal mortality in developed countries. In addition, each year, 700 women die from pregnancy-related complications, and for every death, 70 more come close. Severe maternal morbidity affects 50,000 women annually in the U.S. alone2.
Behind each of these statistics stands a care team burdened by the cognitive overload caused by the tsunami of clinical and operational data. The manager of labor and delivery should ideally be focused on leading their team through life’s most fragile minutes. And yet, staff shortages compound the challenge as documentation requirements consume up to 40 percent of every nursing shift3—time that can be spent with the patient. At the bedside, nurses pivot between compassion and crisis management, chasing real-time data through layers of screens while fetal heart rate interpretation remains a highly manual, subjective task. In the server room, the IT managers maintain aging infrastructure.
And yet when cloud migration appears on the agenda, hesitancy surfaces: Will HIPAA safeguards hold? What if a network outage has a profound impact on the delivery? Such doubts have kept many maternity units tethered to on-prem servers well beyond their shelf life, missing the transformative potential of cloud-native architectures.
CareIntellect for Perinatal: Where cloud meets clinical need
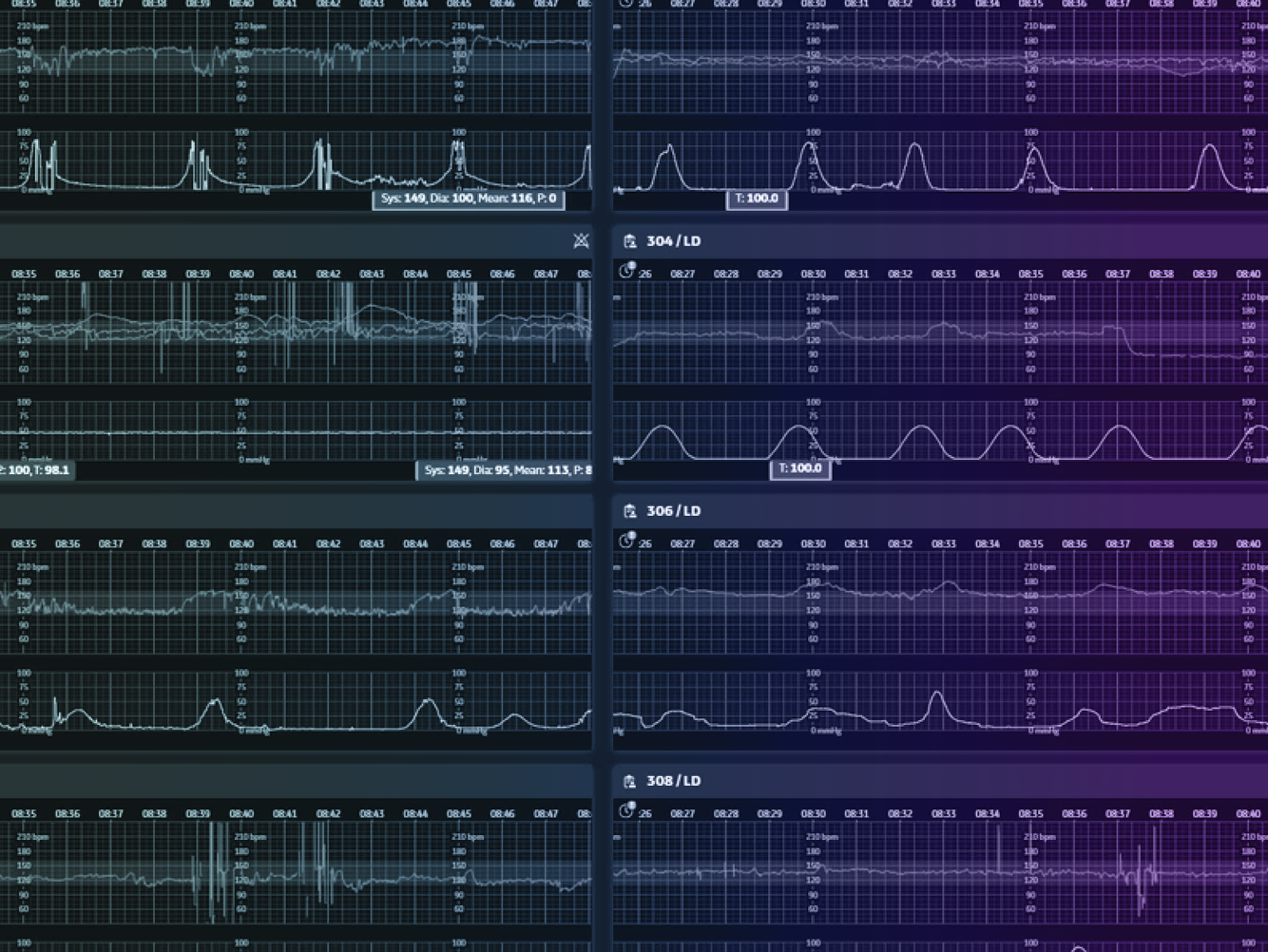
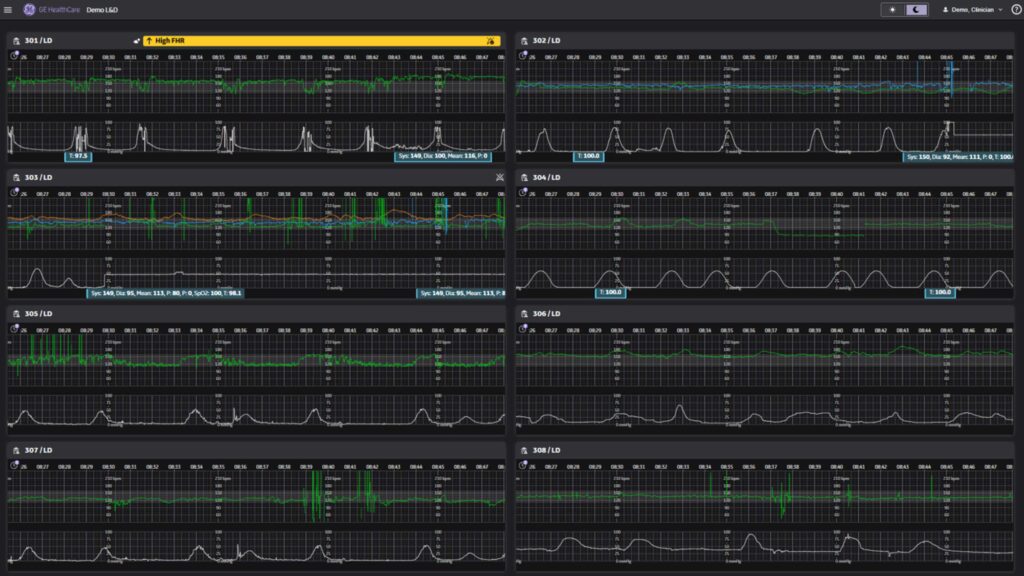
Built on six decades of fetal monitoring expertise and informed by 75 million births and counting, CareIntellect for Perinatal enables maternity units to capture, interpret, and act on clinical data that can generate actionable insights. The application unifies raw waveforms, nursing inputs, and device telemetry into a single view that helps clinicians dial into the significance of every heartbeat.
This transformation requires more than traditional IT infrastructure can deliver. According to studies, a cloud-first architecture on Amazon Web Services (AWS)4 supports HIPAA compliant cloud security that would cost millions to replicate on-prem,[JP1] [AK2] with encryption protecting every data point and dedicated teams monitoring around the clock. When one data center experiences an issue, clinical care can continue seamlessly through automatic failover to other regions. Built on cloud native SaaS solutions, software patches can now be applied in the background to maintain system health and security to avoid impact to day-to-day clinical operations
The advantages extend beyond reliability. Updates can be delivered continuously rather than waiting for annual software releases. Infrastructure operates on a predictable SaaS model based on historical birth volumes, eliminating the need for hospitals to maintain extensive IT resources and on-premise systems. This cloud-based approach stands to dramatically reduce the technical burden on hospital IT teams while ensuring reliable access to critical systems. Rather than managing servers, updates, and scaling challenges internally, hospitals could benefit from enterprise-grade infrastructure through a simple subscription, transforming complex technical operation requiring significant IT staffing into a streamlined service.
Most importantly, this cloud foundation removes the technology barriers that have long frustrated clinical teams. Instead of wrestling with multiple systems and delayed updates, caregivers can better focus on their essential work. CareIntellect for Perinatal seeks to address three fundamental challenges in modern maternity care: achieving clarity from clinical data, ensuring seamless communication across care teams, and maintaining consistent standards across every shift.
1. Enhancing personalized care through clinical precision
A century ago, a midwife relied on intuition and a wristwatch. Today, bedside sensors stream multiple data points a minute: heart-rate variability, contraction frequency, oxygen saturation, and more. And yet insight still hinges on how quickly those signals cohere. The application highlights emerging fetal signs, trends maternal vitals, and surfaces recommendations, helping nurses intervene before trouble sets in.
This clinical precision is only possible through cloud infrastructure. AWS’s elastic compute scales processing power to analyze complex waveforms in real-time with real-time HL7 data feed from all devices. The cloud’s distributed architecture ensures that even during peak census, every heartbeat is captured, displayed, and preserved.
2. Uniting care teams with clarity and confidence
Inter-service and inter-professional handovers face greater challenges than shift-based ones due to differences in clinical expertise, professional backgrounds, and roles between healthcare providers. A prime example is handovers between obstetric nurses and neonatal physicians during high-risk deliveries, which occur in about 10% of US births5, and involve complex safety considerations for both mother and newborn. Each miscommunication carries a price, be it financial, clinical, or human.
CareIntellect for Perinatal creates clarity from confusion. By filtering, prioritizing, and clarifying critical data, the application enhances clinical instincts rather than replacing them. It automates patient trend analysis, integrates practice guidelines, and compiles immediate clinical data from multiple sources into a single, context-aware view—reducing cognitive load and supporting confident, informed decision-making.
Cloud architecture supports more seamless coordination, handoffs and communication possible. For example, AWS’ elastic compute scales processing power to analyze complex waveforms and HL7 data feed from all devices in real-time, whether accessed from bedside tablets or remote monitoring stations.Each clinician has real-time access to the same truth from anywhere in the hospital.
3. Advancing care consistency for every family
Variability is the quiet adversary of obstetrics: practices differ by shift, by unit, even by room. CareIntellect for Perinatal addresses that drift by embedding bias- tested risk models—including Bishop score, shoulder dystocia, and postpartum hemorrhage risk assessments—directly into the patient banner for immediate visibility.
Because CareIntellect for Perinatal runs as a managed service on AWS, updates roll out in weeks rather than fiscal years, letting hospitals adopt new guidelines without ripping and replacing hardware. Capacity scales with census—surging during baby booms, contracting when rooms sit idle—while encrypted backups and multi-site redundancy preserve access even during local outages.
All CareIntellect applications share a common backbone. This can enable hospitals to integrate once and add modules without disruption. Common identity management enabled by integrations with single sign-on eliminates password sprawl, while centralized logging provides unified security monitoring. The coherent interface is aimed to shorten training curves—a nurse who masters perinatal monitoring should be capable of transitioning seamlessly to other use cases easily.
In the delivery room, where seconds matter and do-overs don’t exist, CareIntellect for Perinatal ensures that technology rises to match the miracle it serves. The first cry still silences the unit —but now the chorus of machines that precede this wonderful sound speaks with one voice, clear and true, ready for whatever comes next.
- https://www.acog.org/advocacy/policy-priorities/maternal-mortality-prevention ↩︎
- https://www.commonwealthfund.org/sites/default/files/2021-10/Declercq_severe_maternal_morbidity_in_US_primer_db.pdf ↩︎
- https://www.aacn.org/blog/nursing-documentation-burden-a-critical-problem-to-solve ↩︎
- https://awsforengineers.com/blog/aws-vs-on-premises-cost-analysis-for-modernization/# ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6542453/ ↩︎